For the last 30 years, the idea of a right to die has been widely debated in the U.S.
SAN MARCOS, Texas — In 1993, John Brand, John Lindell, Sally Robinson, and I, along with a couple of others, whose names have faded from my memory, formed an Austin chapter of the Hemlock Society, which was created in 1980 by Derek Humphrey. Our purpose was to learn how to take charge of the end of our lives and to avoid suffering should we be unfortunate enough to be stricken with a debilitating illness from which we would not recover.
We were not a morbid group in the least. In fact, we were jovial, yet thoughtful and determined to make the best of whatever time we had left. I was probably the youngest member, not quite 50 years old. The group — the Austin Hemlock Society — met regularly until 2004, when the national Hemlock Society changed its name to End-of-Life Choices, and then was merged into Compassion in Dying, finally changing its name to Compassion & Choices.
In a later edition of Derek Humphry’s 1991 book Final Exit, he explains how to use inert gas to have a peaceful, effective, and reliable hastened death. The most readily available inert gas at the time was helium, which could be purchased in party balloon kits at Target, Walmart, and other stores. (About six or seven years ago, the manufacturers of the kits began adding about 20% oxygen to the canisters of helium, making the kits unsuitable for our purpose.)
Many people are surprised to learn that taking one’s own life is not against the law.
In 1998, the Austin Hemlock chapter held a public meeting at a local hotel to hear Faye Girsh, the newly-elected president of the national Hemlock Society, speak about Hemlock’s work. Many people are surprised to learn that taking one’s own life is not against the law. What is prohibited in most, but not all, states is helping someone end their own life.
That same year, at Girsh’s urging, Hemlock started a program called “Caring Friends,” which provided trained volunteers to meet with an applicant and teach the person how to hasten their death so that they could avoid suffering or a deteriorating quality of life. The volunteer also was available to be at the person’s side when they died to provide emotional support — a caring friend. The use of inert gas for hastening death began in 1999.
The mergers resulted in dropping the Hemlock name, and the new organization, Compassion & Choices, stopped the Caring Friends program to focus on promoting legislative solutions to aid in dying. When that happened, Girsh, Ted Goodwin, Earl Wettstein, Derek Humphry, and several other Hemlock stalwarts formed Final Exit Network (FEN) to continue the work of Caring Friends under the name Exit Guide Program.
Volunteer medical doctors, psychologists, social workers, and others from all walks of life joined together to establish the program, develop procedures, start a volunteer-training regimen, and build a new organization dedicated to instructing and educating those who wanted to hasten their death because their quality of life had become, or soon would become, unacceptable to them as a result of deteriorating health.
How Final Exit Network operates
The “Guiding Principle” of the nonprofit, volunteer-operated Final Exit Network explains its philosophy:
Mentally competent adults have a basic human right to end their lives when they suffer from a fatal or irreversible illness or intractable pain, when their quality of life is personally unacceptable, and the future holds only hopelessness and misery. Such a right shall be an individual choice, including the timing and companion, free of any restrictions by the law, clergy, medical profession, even friends and relatives no matter how well-intentioned. We do not encourage anyone to end their life, do not provide the means to do so, and do not actively assist in a person’s death. We do, however, support any member who requests it when medical circumstances warrant their decision.
The philosophy of the Final Exit Network is implemented by
- offering free service to all who apply, providing relevant information, home visits if possible and compassionate counseling for the individual and family
- raising the awareness of all Americans concerning this basic human right
- promoting the use of advance directives and other related legal instruments to document the intentions of any individual
- sponsoring research into new peaceful and reliable methods to end life
- vigorously defending “our guiding principle” in a court of law when necessary
Hospice tries to alleviate a patient’s symptoms so that suffering is significantly reduced.
For the last 30 years, the idea of a right to die has been widely debated in the U.S. Most people who make use of this right do so by refusing ultimately futile medical treatment or procedures. Often they are aided by hospice, which began in the U.S. in New Haven, Connecticut, in the early 1970s, and became widespread by the early 1990s. Generally, hospice follows a philosophy that focuses on palliative care of a terminally ill or dying patient’s symptoms, whether physical, emotional, spiritual, or social. Rather than focus on treatment, hospice tries to alleviate a patient’s symptoms so that suffering is significantly reduced or eliminated. For some people, however, palliative care is ineffective in relieving their suffering or does not meet their other needs, and they seek to end their lives rather than continue suffering.
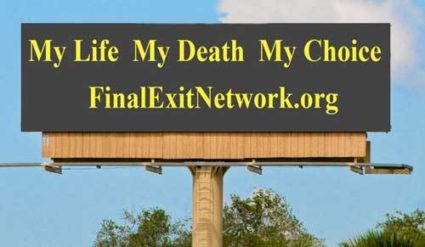
Perhaps the most important aspect of aid in dying, death with dignity, hastened death, physician-assisted suicide, or self-deliverance — whatever one prefers to call it — is that it is the individual’s decision to proceed in such a fashion. No one has the right to actively assist a person to end the person’s own life, encourage such behavior, or promote it in most states. And that focus on each individual’s decision is made clear by the Final Exit Network’s early billboard campaign — “My Life My Death My Choice” — which is intended to promote one’s autonomy in such decisions and encourage thoughtful discussion about the end of life.
Volunteer work with FEN
The Austin Hemlock Society chapter ceased operations after Compassion & Choices was created. Many of us joined FEN soon after it was organized. Beginning around 2014, I began doing volunteer proof-reading for the FEN Newsletter editor. In 2016, I submitted an application to become an Associate Exit Guide, which was accepted, and I was trained with about a dozen other volunteers. Soon thereafter, I was asked to interview an applicant for exit guide services and write a report of the structured interview to be sent to FEN’s Medical Evaluation Committee (MEC), a team of three volunteer doctors who determine whether the applicant satisfies FEN’s requirements for exit guide educational and training services.
A few months later, I was asked to serve as a Coordinator for a multi-state area, returning phone calls from people seeking exit guide education and training. Coordinators explain the Exit Guide program, receive medical records from applicants, arrange interviews for them with other volunteers, prepare application packets to go to the MEC, and arrange for exit guides after a person’s application has been approved.
In 2017, I was approached by Gary Wederspahn, the FEN board member in charge of outreach, about starting a blog for FEN to focus on end-of-life and right-to-die issues. For three years, I edited and moderated the blog — The Good Death Society Blog — writing about 80% of the weekly posts and publishing guest writers when they could be found. The blog is searchable and discusses virtually every issue that concerns the right to die and other end-of-life issues.
I transferred responsibility for the blog to Kevin Bradley at the the end of July. He is a writer, speaker, stress-management counselor, and ordained chaplain who has experience as both a hospital and hospice chaplain. He is an Associate Exit Guide, a member of FEN’s Board of Directors and participates in FEN’s Speakers Bureau. He also provides spiritual counseling to FEN clients, families, and volunteers upon request.
FEN controversies
FEN’s history since 2004 has not been without controversy. In early 2009, prosecutors in Arizona brought charges against four members of the Final Exit Network for allegedly assisting in the death of one individual. One of the accused pleaded guilty to a minor misdemeanor, and none of the other three individuals was convicted of any crime. In Georgia in 2009, four FEN volunteers were similarly charged, and about half of Final Exit Network’s assets were seized under a racketeering law. FEN successfully defended the volunteers and later had all of the seized funds returned.
Assisting a suicide was filed against FEN and several of its volunteers in Minnesota.
A case charging assisting a suicide was filed against FEN and several of its volunteers in Minnesota after the Georgia Bureau of Investigation in 2010 notified law enforcement authorities in Minnesota that it had found documents showing that FEN, then incorporated as a Georgia nonprofit organization, had provided “exit services” to Doreen Dunn at her request in 2007.
In May 2015, FEN was convicted in Minnesota of assisting in the 2007 suicide of Doreen Dunn. In that state, “assisting” does not require any physical act. The Minnesota Supreme Court decided that if speaking to another person about how to commit suicide “enables” that person to take their own life, the speech meets the definition of “assist” as found in the Minnesota statute that prohibits “assisting suicide.” FEN paid a fine of $30,000, the maximum under the law, and was unable to have the conviction overturned on appeal. None of the FEN volunteers involved in the case were subsequently prosecuted.
The Minnesota “Assisted Suicide” law, as interpreted by the state supreme court, renders free speech in Minnesota the most limited right imaginable. State prosecutors told the Court of Appeals of Minnesota that if someone walks into a library in Minnesota and says to the librarian, “I am ready to die. Can you show me where to find this library’s copy of Final Exit?” the librarian would commit a felony if she showed the patron where to find Derek Humphry’s book, and the patron then ended her own life using inert gas as described in the book.
FEN volunteers do not physically assist anyone to end their own life.
FEN volunteers do not physically assist anyone to end their own life. The volunteers train and educate clients about how to hasten their own deaths using inert gas. Each client must be capable physically of carrying out the procedure, and must be mentally competent. Exit Guides are usually available to provide a “compassionate presence,” but not assistance, when a person decides it is time to die.
FEN’s eligibility criteria
Although FEN does not require a client to have a terminal illness to be eligible for its services, it does require mental competency at the time of application for education and training services and at the time the person chooses to exit. But in addition to the mental competency criterion, FEN requires that applicants
- have “existing or reasonably anticipated unbearable suffering or an unacceptable or intolerable quality of life with no reasonable hope of improvement”
- be aware of treatment options, “though applicants are not required to pursue treatment that is unacceptable to them”
- demonstrate that they have informed, or expressed “a willingness to inform, close family members and intimate associates of the applicant’s intent”
- submit a personal statement describing “how the medical condition meaningfully reduces or will reduce the applicant’s quality of life, including examples of current physical or mental decline, . . . the applicant’s values as they pertain to end-of-life choices, and a statement of what the applicant wants from Final Exit Network.”
Specific criteria of FEN’s program
In addition to meeting all the general criteria, an application must fall into at least one of the following four categories [the specific criteria]:
- Serious Physical Disease: The applicant’s medical records must confirm a diagnosis of a recognized, serious disease that is evident on physical examination, imaging studies, or laboratory tests. Examples include, but are not limited to, all forms of malignancy; hereditary and acquired neurological conditions such as Huntington’s disease, multiple sclerosis, and amyotrophic lateral sclerosis; disabling cardiovascular disease; and progressive pulmonary disease.
- Chronic, Severe, Somatic Pain: The applicant’s medical records must confirm that the applicant experiences chronic, severe, uncontrolled pain; . . . medical records must show evidence of the severity, duration, and intractable nature of the pain despite reasonable medical attention, although this evidence may only be documentation of the applicant’s chief complaints and exclusion of possible causes.
- Dementia: The applicant’s medical records must confirm a diagnosis of cognitive impairment or dementia and provide evidence based on cognitive or neurological test results. The dementia may be a progressive type, such as Alzheimer’s, or a stable type, such as dementia from a stroke.
- Constellation of Conditions: The applicant’s medical records must confirm that the applicant suffers from a combination of irreversible medical conditions. This category is intended to capture what is sometimes called “completed life,” “life well lived,” or “old age rational suicide,” but may also include a constellation of medical conditions resulting from an intractable chronic condition, such as diabetes or an autoimmune disorder.
Voluntarily Stopping Eating and Drinking (VSED)
FEN supports one other method of hastening death — voluntarily stopping eating and drinking (VSED). It is another way to have a good death that is often assisted by hospice. VSED frequently occurs naturally near the end of a disease, or it can be intentionally pursued to avoid lingering, sometimes for years. With VSED, dehydration causes the body to shut down. Death usually occurs within seven to 10 days or so after VSED begins.
FEN has developed a special supplemental directive designed for those who have dementia.
FEN has developed a special supplemental directive using VSED and designed for those who have dementia, but who want to live only as long as the disease leaves them with some enjoyment in living or recognition of who they are.
FEN’s dementia directive begins with listing the physical and mental conditions that will be used to determine when the directive is triggered — what the directive terms “My Chosen End Point.” When that point is reached, the directive provides for receiving “the best available palliative care,” for receiving no medical treatment for conditions that could lead to death, and directs the beginning of voluntarily stopping eating and drinking (VSED). In addition, it provides for no revocation of the directive, giving one’s health care surrogate the duty only to determine when the end point has been reached. It also provides that any health care institution caring for the person accept the terms of the directive or make provisions for it to be implemented.
The legal status of such a directive has not been tested in courts, but will be legally supported by FEN should that be necessary, at no cost to the person executing the directive, provided they are accepted into the project by FEN at the time of execution of the directive. Litigation may be the only recourse to have the dementia directive implemented. Because there are no definitive nationwide court decisions regarding following VSED instructions written when one was still mentally competent, on behalf of one’s future demented self, the decision by FEN to offer to litigate the issue at no cost to the patient or family is unique.
FEN’s dementia directive can be found here. To take advantage of FEN’s offer of legal representation, send an email to fenattorney@gmail.com and indicate your interest.
Conclusion
Obviously, not everyone will need or want to end their own life before it comes to a natural end. We won’t all need medical assistance in dying or inert gas to have a good death. But many of us who have experienced a family member or friend with dementia or Parkinson’s or ALS or cancer, or some other condition which makes a good death difficult or impossible, often remark that we don’t want our own lives to end that way. Most of us will die quickly of a heart attack, or in our sleep, or by misadventure. Still others will find the help of hospice to be an essential ingredient in having a good death. But many of us may want to take matters into our own hands, with the help of a clinician or the advice and counsel of FEN.
Unlike medical assistance in dying (MAID), which is available in only ten US jurisdictions (Montana by judicial decree, and by law in Oregon, Washington, Vermont, Maine, District of Columbia, Colorado, California, Hawaii, and New Jersey), FEN operates throughout the country, responding to the suffering of people who have a debilitating illness from which they will eventually die. FEN’s application process is comprehensive, and yet available to far more people than MAID, and is requested often in those jurisdictions that have MAID laws.
The work that FEN does demonstrates that, with appropriate safeguards, it is possible to take control of one’s life and end or avoid additional suffering when facing a debilitating or irreversible illness. Helping people in distress at the end of their lives is often challenging for both FEN’s volunteers and clients, but it has been among the most rewarding work I have ever done, and the people who are helped are invariably grateful. Their gratitude seems tied to their desire to exercise that final freedom–the freedom to control the quality of their lives, avoid suffering, and determine the manner and timing of their deaths.
[Rag Blog columnist Lamar W. Hankins, a former San Marcos, Texas, City Attorney, is retired and volunteers with the Final Exit Network as a coordinator for people in seven states and serves as editor, contributor, and moderator of The Good Death Society Blog, which discusses a wide range of end-of-life issues.]
- Read more articles by Lamar W. Hankins on The Rag Blog.