At last the incurably traumatised may be seeing the light at the end of the tunnel.
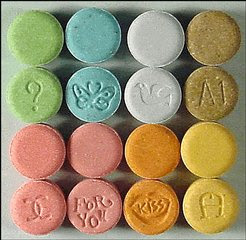
And controversially, the key to taming their demons is the ‘killer’ drug Ecstasy
By Amy Turner
The following story was originally posted on May 4, 2008 in the Times of London. It’s an eye opener.
An Ecstasy tablet. That’s what it took to make Donna Kilgore feel alive again – that and the doctor who prescribed it. As the pill began to take effect, she giggled for the first time in ages. She felt warm and fuzzy, as if she was floating. The anxiety melted away. Gradually, it all became clear: the guilt, the anger, the shame.
Before, she’d been frozen, unable to feel anything but fear for 10 years. Touching her own arms was, she says, “like touching a corpse”. She was terrified, unable to respond to her loving husband or rock her baby to sleep. She couldn’t drive over bridges for fear of dying, was by turns uncontrollably angry and paralysed with numbness. When she spoke, she heard her voice as if it were miles away; her head felt detached from her body. “It was like living in a movie but watching myself through the camera lens,” she says. “I wasn’t real.”
Unknowingly, Donna, now 39, had post-traumatic stress disorder (PTSD). And she would become the first subject in a pioneering American research programme to test the effects of MDMA – otherwise known as the dancefloor drug Ecstasy – on PTSD sufferers.
Some doctors believe MDMA could be the key to solving previously untreatable deep-rooted traumas. For a hard core of PTSD cases, no amount of antidepressants or psychotherapy can rid them of the horror of systematic abuse or a bad near-death experience, and the slightest reminder triggers vivid flashbacks.
PTSD-specific psychotherapy has always been based on the idea that the sufferer must be guided back to the pivotal moment of that trauma – the crash, the battlefield, the moment of rape – and relive it before they can move on and begin to heal. But what if that trauma is insurmountable? What if a person is so horrified by their experience that even to think of revisiting it can bring on hysterics? The Home Office estimates that 11,000 clubbers take Ecstasy every weekend. Could MDMA – the illegal class-A rave drug, found in the system of Leah Betts when she died in 1995, and over 200 others since – really help? Dr Michael Mithoefer, the psychiatrist from South Carolina who struggled for years to get funding and permission for the study, believes so. Some regard his study – approved by the US government – as irresponsible, dangerous even. But Mithoefer’s results tell a different story.
MDMA was patented in 1912 by the German pharmaceutical company Merck. To begin with, it was merely an intermediate chemical used in creating a drug to control bleeding. In the 1920s MDMA was used in studies on blood glucose as a substitute for adrenaline. The Merck chemist Max Oberlin concluded that it would be worth “keeping an eye on this field”. Still, no further studies were carried out until 1952, when the chemist Dr Albert van Schoor tested the toxicity of MDMA on flies. “Flies lie in supine position, then death,” he recorded.
MDMA’s therapeutic potential wasn’t realised until 1976, when the American chemist Alexander Shulgin tried it on himself. He noted that its effect, “an easily controlled altered state of consciousness with emotional and sensual overtones”, could be ideal for psychotherapy, as it induced a state of openness and trust without hallucination or paranoia. It quickly became known as a wonder drug, and began to be used widely in couples therapy and for treating anxiety disorders. None of these tests was “empirical” in the scientific sense – no placebos, no follow-up testing – but anecdotally the results were almost entirely positive.
Word, and supplies, of the new “love drug” got out, and in the early 1980s it became popular in the fashionable clubs of Dallas, LA and London, where it was known as Ecstasy, X or “dolphins”. As use became widespread, the US authorities panicked, and by 1985 MDMA was an illegal, schedule-1 drug. UK laws were even tighter: MDMA, illegal under the 1971 Misuse of Drugs Act, was categorised class A in 1977, carrying a sentence of up to seven years for possession.
Criminalisation put paid to MDMA research almost overnight, at least until Mithoefer’s current programme began. But it didn’t stop the ravers. The drug was popular in the late 1980s and early 1990s for its energising, euphoric effects. There are no official figures for that period, but the Home Office estimates that in 2006/7, between 236,000 and 341,000 people took Ecstasy. Experts say the drug is far less fashionable now than in its heyday in 1988, the second so-called “summer of love”.
The MDMA used in the studies – the drug Dr Mithoefer gave Donna and other patients – was the pure chemical compound, not the black-market Ecstasy bought by recreational users. “A lot of Ecstasy pills aren’t MDMA at all,” says Steve Rolles of the drug-policy reform group Transform. “They may be amphetamines, or unknown pharmaceuticals, or they can be cut with almost any drug in pill or powder form. That’s when you magnify risks associated with taking a drug that’s already toxic. Plus, people use it irresponsibly, mixing it with other drugs, not drinking enough water or drinking too much.”
The images of Leah Betts and Lorna Spinks lying in hospital on life-support, bloodied and bloated, are familiar to all of us – we know drugs cost lives. But has MDMA’s reputation been tarnished so badly that its potential medical value has been overshadowed? That question is the reason that Donna agreed to speak to The Sunday Times about her MDMA treatment. “It’s so important people know what it did for me, what it could do for others,” she says. Her voice trembles: it isn’t easy to talk about what she went through.
In 1993, Donna was brutally raped. She was a single parent living in a small town in Alaska, working as a dental nurse for the Air Force. She was due to work an early shift the next day and her two-year-old daughter was staying with a friend for the night. She was alone at home. At midnight she opened the door to a stranger who said he was looking for his dog. He asked if her husband was at home, and a second’s hesitation was enough. He burst in, backing her up against the fireplace in the living room. Donna picked up a poker to defend herself. He said: “If you co-operate, I won’t kill you. I’ve got a gun.” And he reached into his jacket.
“I dropped the poker and that was it,” she says. “I thought, this is how I’m going to die. No life flashed before my eyes, I didn’t think about my daughter. Just death. I left my body and I stayed that way. The next thing I remember, the cops were coming through the door with a dog.”
She endured the rape with her eyes squeezed shut. That she hadn’t physically struggled would later form a large part of the guilt and shame that contributed to her PTSD. “I guess a lot of women would say, ‘Someone would have to kill me before I’d let that happen.’ Well, I did what I thought I had to do to survive,” she says. When she heard a shuffle of feet outside the door she screamed for all she was worth. Her attacker beat her. Two policemen, probably alerted by a neighbour, broke down the door and arrested the man, then drove Donna to the Air Force hospital where she worked. “Of course it was full of people who knew me,” she says. “It was completely embarrassing. And after that, nobody knew what to say. People avoided me, they looked at me funny. It was miserable.”
Afterwards, convinced that getting on with life was the best thing for herself and her child, Donna carried on as usual. She was embarrassed that people who knew her also knew about the rape, particularly as she was still working at the hospital. But she couldn’t remember much of the attack itself, and didn’t try. So she was surprised when, four years later, her symptoms started to kick in. “I had no idea it was PTSD. I couldn’t understand why I was so angry, why I was having nightmares, flashbacks, fainting spells, migraine, why I felt so awful, like my body was stuffed with cotton wool. Things had been going so good.”
She started drinking heavily and went from relationship to relationship, finding men hard to trust and get close to. Convinced that she was dying and wouldn’t live to see her next birthday, she went to the Air Force psychiatrist. “And that’s where it started – take this pill, that pill. I’ve been on every kind of antidepressant – Zoloft, Celexa, Lexapro, Paxil. Wellbutrin made me feel suicidal. Prozac did the same. The pills were just masking the symptoms, I wasn’t getting any better.”
Yet she met her “soul mate”, Steve, and married him in 2000. “When I first saw him I thought, ‘This is the man I’m going to spend the rest of my life with.’ We were like one person, finishing each other’s sentences,” she says. They muddled along, with Donna putting on a brave face. She had two more children. But getting close wasn’t easy: “The longer we were married, the worse I got.”
Once, Steve and Donna were watching TV when she had a vivid flashback to the night she was raped. “I looked at the door, I saw it open, and that feeling came over me all over again.
I thought, ‘My God, why won’t this go away?’ Steve tried to understand, but unless you’ve been through this, you don’t know what it’s like.”
Donna moved to South Carolina in 2002 when Steve – also in the services – was posted there. She began seeing a psychiatrist called Dr Marcet, who diagnosed her with PTSD and attributed it to the rape. It helped to know that whatever it was had a name and a cause: “I was like, why hasn’t anybody told me this before?” It was Marcet who referred her to the Mithoefers.
Donna had never taken Ecstasy before. “I was a little afraid, but I was desperate. I had to have some kind of relief. I didn’t want to live any more. This was no way to wake up every morning. So I met Dr Mithoefer. I said, ‘Doctor, I will do anything short of a lobotomy. I need to get better.’ ” That’s how, in March 2004, Donna became the first of Mithoefer’s subjects in the MDMA study. Lying on a futon, with Mithoefer on one side of her and his wife, Annie, a psychiatric nurse, on the other, talking softly to her, she swallowed the small white pill. It was her last hope.
“After 5 or 10 minutes, I started giggling and I said, ‘I don’t think I got the placebo,”’ she recalls. “It was a fuzzy, relaxing, on-a-different-plane feeling. Kind of floaty. It was an awakening.” For the first time Donna faced her fears. “I saw myself standing on top of a mountain looking down. You know you’ve got to go down the mountain and up the other side to get better. But there’s so much fog down there, you’re afraid of going into it. You know what’s down there and it’s horrible.
“What MDMA did was clear the fog so I could see. Down there was guilt, anger, shame, fear. And it wasn’t so bad. I thought, ‘I can do this. This fear is not going to kill me.’ I remembered the rape from start to finish – those memories I had repressed so deeply.” Encouraged by the Mithoefers, Donna expressed her overwhelming love for her family, how she felt protected by their support and grateful for their love.
MDMA is well known for inducing these compassionate, “loved-up” feelings. For Donna, the experience was life-changing.
So what happened when she went home? Was she cured? She sighs. “I don’t know if there’s such a thing as a cure. But after the first session I got up the next day and went outside, and it was like walking into a crayon box – everything was clear and bright. I did better in my job, in my marriage, with my kids. I had a feeling I’d never had before – hope. I felt I could live instead of exist.”
What makes MDMA so useful, Mithoefer believes, is the trust it establishes. “Many people with PTSD have a great deal of trouble trusting anybody, especially if they’ve been betrayed by someone who abused their trust, like a parent or a caregiver,” he says. “MDMA has this effect of lowering fear and defences. It also allows more compassion for oneself and for others. People can revisit the trauma, feel the original feelings but not be retraumatised, not feel overwhelmed or have to numb out to cope with it.”
Before they can take part in Mithoefer’s study, every participant undergoes rigorous testing. There are 21 participants per phase and the study is now in its second phase. First, they must be diagnosed with PTSD. Then its severity is measured on the Clinician Administered PTSD Scale (Caps) – it must be at least “moderately severe”. They must be “treatment-resistant”, meaning they have failed to respond to at least one other type of psychotherapy and also drug treatment with an SSRI (selective serotonin reuptake inhibitor) antidepressant. They must sign a 20-page document giving informed consent; they cannot have an addiction, psychosis or bipolar disorder, because these conditions affect the ability to give consent. Then they have a physical examination, a full medical-history check and lab tests for cardiovascular disease.
After the screening, the patient has two 90-minute “preparatory sessions” with the Mithoefers, to begin to build trust and get an idea of what may lie ahead. “We make sure they understand that symptoms will be stirred up, that painful feelings will come before they feel better and that they should experience them as fully as they can, and express them, rather than blocking them out,” Mithoefer says. “We have one rule: during the session they don’t have to talk at all if they don’t want to, or they can talk about anything they feel like. But if, after an hour, the trauma topic hasn’t come up, we can bring it up. But it always does come up,” he chuckles.
The patient lies on the futon in the Mithoefers’ living-room-style office in Charleston, South Carolina. They wear eye shades to encourage introspection, and headphones through which relaxing music is played. Annie keeps an eye on the blood-pressure cuffs and temperature gauge. Mithoefer sits opposite, taking notes. Each patient is given a recording of their session afterwards.
The patient takes either a 125mg tablet of MDMA or a placebo pill, followed by a 62.5mg dose about two hours into the therapy session. The study is double-blind, so only the emergency nurse who carries the drugs from the safe to the office knows whether the patient is getting the drug. “We can always tell whether it’s real or placebo. The patient can’t – some people thought they got MDMA when they didn’t,” says Mithoefer. “But we’re seeing very encouraging results. There’s a real difference between placebo patients and patients who got MDMA, in terms of their ability to relive the trauma.”
Michael and Annie Mithoefer “aren’t your typical kind of therapists”, says Donna. She was dubious about Michael’s ponytail and sandals when they first met, but she is emotional as she talks about him now. “I don’t think I’ve ever met two people who cared so much about people getting well. I’d see tears in their eyes when I told them what I went through.” Three other former patients of the Mithoefers who contacted me about this article described them as “heroes”, “pioneers”, even “life-savers”.
At the time the Mithoefers treated Donna, in March 2004, their study had been a long time in the pipeline. Convinced of MDMA’s potential, Rick Doblin, founder of the Multidisciplinary Association for Psychedelic Studies (Maps), had been in and out of the courts seeking permission from the Food & Drug Administration for clinical research since 1984. Maps, a group set up to fund psychedelic research, agreed to fund Mithoefer’s study in 2000. The next year the FDA approved it. Then approval was withdrawn because of research by the neurologist George Ricuarte, at Johns Hopkins University, claiming that MDMA was lethally toxic. Even a single use, he reported, could cause brain damage and possibly Parkinson’s disease. Ricuarte retracted his findings in 2002 when it turned out that bottles had been mixed up and the monkeys used as subjects had received lethal doses of methamphetamine (speed), rather than MDMA. “It was incredibly frustrating,” Mithoefer says.
Mithoefer’s study, which looks set to cost $1m by the time it finishes in four years’ time, is scrupulously monitored. Doblin had 1,000g of MDMA made specially, each gram costing $4. Mithoefer had to obtain a licence from the Drug Enforcement Administration (DEA), which keeps track of exactly how much MDMA each licence-holder has, and periodically checks the stocks for purity. A defibrillator must be kept in the building at all times in case of cardiac arrest, and an emergency nurse must be present during the treatment session. Once the study is complete, it will be subject to peer review. Then, all being well, Mithoefer hopes to see MDMA therapy available on prescription, administered in controlled surroundings, in 5 to 10 years.
Interest is growing in the UK too, but scientists admit it will take time to change hearts and minds. Dr Ben Sessa of Bristol University’s Psychopharmacology Unit has been writing papers on MDMA therapy for two years. “The Mithoefers’ struggle has been ludicrous,” he says. “There’s plenty of anecdotal evidence that it could be really useful in psychotherapy. There they are, qualified doctors with experience and medical backup, giving people this tiny dose of MDMA with safeguards in place. It took them 20 years for Maps to get it off the ground and it costs $1m. The irony is that thousands of people are taking this stuff every weekend and there’s a 15-year-old on the street corner who’ll sell it to you for a tenner.”
Sessa would like to set up a programme of research in the UK, pointing to the thousands who could benefit: “For severe, unremitting PTSD sufferers, it could be a lifeline. What they’re seeing in the US is people who have suffered for years suddenly saying, ‘Wow, for the first time in my life I can talk about this, I can live with it.’ And these are not young ravers. They’re people in their thirties, forties, fifties who have never taken drugs. It’s quite remarkable.”
But what about the potential for post-study abuse? Might someone who felt deflated after the elation of their MDMA session find the urge to self-medicate irresistible and pop to that 15-year-old on the corner for a quick fix? Not at all, says Sessa. “I prescribe Valium all the time, and when the course is finished the patient could go and buy Valium on the street, but they don’t. Very few people are interested in recreational drugs.”
I ask Donna the same question. “Would I take the drug again? Yes, definitely,” she says. “But not without a therapist. It’s illegal.”
Another former patient of Mithoefer’s, a 42-year-old woman, had severe PTSD after being repeatedly and horrifically beaten and locked in a basement by her father during childhood. She wished to remain anonymous because she is still in contact with her parents. When I asked her the question, she replied: “I did it to get better, not to get high. Before the treatment, I would drink to hide my symptoms. But I don’t want to get drunk now, let alone take drugs. I just don’t need it any more.”
The harmful effects of MDMA are still under investigation. The type of research that is carried out – normally with animals or with recreational users who also take other drugs – means that the exact levels of toxicity it causes are unknown. In 2006 Dr Maartje de Win of the University of Amsterdam published research showing that Ecstasy could cause depression, anxiety and long-term memory damage after one small dose. “We really don’t know how much Ecstasy affects the brain in the long term,” she says. “I would be very cautious about giving it therapeutically. We need to conduct much more research. And even then it should only be given as a last resort, after weighing the benefits against the risk of harm.”
Sessa is adamant that research into MDMA is justified. “Look at heroin. It’s a class-A drug that’s dangerous when used recreationally, but it’s used widely in medicine, and so it should be – it’s a very useful drug. Can you imagine saying to the Royal College of Anaesthetists, ‘You can’t use morphine or diamorphine [heroin] or pethidine or codeine or any opiate-based drugs because heroin is dangerous and people abuse it?’ It’s culturally bound. MDMA has been demonised.”
In 2004, the most recent year for which there are records, 46 people died after taking Ecstasy, as against 8,221 alcohol-related deaths. And most of those who die with MDMA in their system have mixed it with substances such as alcohol or cannabis, which confounds the picture.
Earlier this year, the police chief for North Wales, Richard Brunstrom, called for the drug to be reclassified, claiming it was “safer than aspirin”. He was widely shouted down, but Steve Rolles of Transform believes he may have a point. “It’s not appropriate to have Ecstasy in class A. In terms of indicators of harm – toxicity, mortality, addictiveness and antisocial behaviour – it’s not comparable to heroin or cocaine. But the government won’t reclassify it. Reclassifying cannabis [from class B to C] in 2004 caused years of grief from opposition parties and the media.”
The minister for drugs policy, Vernon Coaker, declined to comment on reclassification for medical purposes, but a spokesman said: “The government has no intention of reclassifying Ecstasy. It can and does kill unpredictably; there is no such thing as a ‘safe dose’. We firmly believe it should remain a class-A drug. In addition, the government warns young people of the dangers of Ecstasy through the Frank campaign.”
It does. But it also gives advice on safe Ecstasy use – or “harm minimisation”. This is precisely the mixed message that Rolles believes is damaging. “Harm reduction is reducing the harm that’s created by illegal supply in the first place,” he says. “So you have harm-reduction information within a legal framework that maximises harm. It’s a clear contradiction.”
Then there is the problem of funding. MDMA therapy is based on the idea of a single treatment, or a course of treatment sessions, rather than long-term prescriptive use. This presents little or no benefit to drug companies that have huge budgets for research as long as there’s a saleable product at the end. And if MDMA does prove effective, companies could stand to lose millions from lost sales of long-term antidepressants prescribed for PTSD.
Sessa says: “There’s no financial incentive for the pharmaceutical companies to look into it. Psychotherapy is notoriously underfunded and discredited by the drug companies. It could benefit the government to look into MDMA, but their funding is a drop in the ocean next to a company like Pfizer’s research budget. So who’s going to pay for a multi-centre psychotherapy trial for 10,000 people – the couch-makers?”
PTSD therapy currently costs the NHS £14m a year, and with more veterans returning from Iraq and Afghanistan, that figure is set to rise. Last year, 1,200 new veterans sought treatment for PTSD from the organisation Combat Stress, compared with 300 in the year 2000. But realistically, would the government ever sanction MDMA research? “It’s not impossible, but it’s improbable,” says Sessa. “It takes a very brave politician to look at the evidence and say, ‘Well, there might be positive aspects to this class-A drug. Let’s look into it.’ It’s a conceptual, social battle which won’t be easy to win.”
Source. / Times of London
Thanks to telebob / The Rag Blog / Posted June 27, 2008
















I have said that LSD saved my life, and I still say it and always will. My early family life was often about blood (My mama’s) and tears (mine); I lived in constant fear of my Father’s unpredictable rage, which was finally ended when another man and his friends showed up with guns and put him in his place. The institution I went into at age four allowed, even encouraged a Lord of the Flies society among the boys. We existed within a heirarchy of meanness and brutality; on vacations up at my Grandma’s place I witnessed yet more life-threatening violence. By the time I was a teenager I recognized that I was different from everyone I met. Cold, aloof, and unnaturally insensitive, I was not really alive. I felt nothing, mistrusted everyone, and hated anyone who seemed the least bit happy; in the last High School I attended, I was known for confronting and tormenting Hippies. The United States Marine Corps seemed the right place for me. My first night on LSD, a hit I had stolen from another Marine, changed everything. I became a “Freak” and a War Resistor and a few months later was discharged from The Marines as a Conscientious Objector.
Praise the Lord and pass the mescaline.
Doug Zachary
I believe that psychedelics have saved many of us from madness. By opening our eyes, like it or not, to the interconnectedness of Being, and to our own Godhead status, means you can no longer cut yourself any slack in the mental preparedness department. We can no longer pretend we don’t know what we’re thinking! Yes, I know that other sweet souls have not been able to take the revelation, and the contradiction with social expectation, and some of them have gone way around the bend where I’ve just peeked around the corner. But maybe the events of the past 40 years would have put them on the funny farm anyway, and maybe those of us who were able to enjoy ego death and come back for more, on a judicious basis, were inoculated against worse outcomes.
The trauma of birth affects us all, apparently, and subsequent events can either make things worse or make them better, but that bottom-line separation and self-consciousness has to get its comeuppance before we can see clearly again through the rose-colored glasses of Creation Unfinished!
If ecstasy works so much better, you might as well just give weed a try…or Jesus (as in Hey Zeus, the son of the imaginary Greek God Zeus who acted like the worst human being imaginable who came down and knocked up teenage girls of antiquity of questionable intelligence and/or character…well, maybe that last one isn’t that great after all at the end of the day.)